Burn-derived Mesenchymal Stem Cells in Wound Healing
Roohi Vinaik1, Marc G. Jeschke1,2,3,4*
1Sunnybrook Research Institute, Toronto, Canada
2Department of Surgery, Division of Plastic Surgery, University of Toronto, Canada
3Department of Immunology, University of Toronto, Canada
4Ross Tilley Burn Centre, Sunnybrook Health Sciences Centre, Toronto, Canada
Abstract
Thermal injury is a severe form of trauma that is accompanied by significant, persistent metabolic and immune dysregulation. The extent of altered post-burn metabolism and inflammation is correlated with severity of injury, with severe burns demonstrating a more significant hypermetabolic, hyperinflammatory response. This in turn delays re-epithelialization and exacerbates poor post-burn wound healing, which is the most important factor in patient mortality outcomes. Recently, stem cells have gained interest in burn wound healing applications due to their capacity to produce multiple cellular subtypes and improve the rate and quality of healing. Here, we focus on applications of mesenchymal stem cells in wound healing. In particular, we highlight the characteristics and efficacy of burn-derived mesenchymal stem cells (BD-MSCs), which improve healing in animal models. Discarded burn tissue is a source of pro-healing BD-MSCs, providing a safe, non-invasive therapeutic option for burn patients.
Burn-Related Complications and Current Standard of Care
Persistent inflammatory derangements are a hallmark of burn trauma that ultimately influences wound healing1. Inflammatory mediators such as cytokines recruit immune cells (e.g. macrophages, leukocytes) to the site of injury during the preliminary stage of wound healing. These cytokines in turn recruit keratinocytes and activated fibroblasts to the wound bed, promoting re-epithelialization, which is a key factor in patient outcomes2-5. However, while inflammation is likely necessary for healing, excessive, prolonged post-burn inflammation in turn promotes tissue destruction and increases risk of abnormal scarring (e.g. hypertrophic scars)6-10. Targeting inflammation with systemic anti-inflammatory agents such as glucocorticoids is detrimental, especially in large burns. Instead, excision and grafting during the inflammatory phase is performed in order to mitigate inflammation and decrease infection, which is another common complication of burn wounds. Burn patients are susceptible to drug resistant infections, which can result in an enhanced immune response accompanied by septic shock, hypotension and poor skin perfusion which ultimately further delays wound healing11. Thus, therapeutic strategies that regulate local immune responses to enhance healing are key in preventing scarring and infection.
Standard of care for burn wound management is early excision and debridement (within 72 hours post-injury) followed by autologous split-thickness skin grafting12-16. Early excision is associated with decreased blood loss, infection and mortality coupled with increased graft take17-20. However, this poses certain challenges, including creation of a new wound site and complications such as pain, scarring, infection21,22. This is in addition to the fact that severe burns (>30% TBSA) require a significant amount of healthy skin for grafting, precluding use of this strategy. Due to these limitations, there is a need for alternative wound coverage strategies, although current options are ineffective secondary to high cost, poor efficacy, and long production time23,24.
Currently, cell-based techniques for permanent coverage are gaining popularity. Culture-based options include patient-derived keratinocyte isolation and expansion into epidermal autografts, which limits the amount of donor skin need for coverage of large burns. However, keratinocyte-based techniques should be employed carefully since hyperactivation may contribute to pathological scarring25. Alternatively, utilizing adult MSCs isolated from bone marrow, hair follicles, adipose tissue, or skin is another viable option. These stem cells promote healing likely via immunomodulation and paracrine activation of host cells, and we discuss characteristics of MSCs in the following section26.
Characteristics of Mesenchymal Stem Cells
MSCs are classified based on characteristics such as plastic adherence, expression of specific cell surface markers (CD73, CD90, CD105) and lack CD14, CD34, CD45 and HLA-DR, and the ability to differentiate in vitro into either adipocytes, chondrocytes or osteoblasts27. While the aforementioned characteristics are applicable to all MSCs, there are slight variations depending on the tissue of isolation. MSCs have several beneficial features for skin regeneration such as the capacity for self-renewal, ability to home towards wounds, rapid proliferation and the ability to differentiate into a host of cell types28. Importantly, their pro-healing effects can be attributed in part to release of growth, cell recruitment, and immunoregulatory factors in response to inflammatory mediators that accumulate at the site of injury – a process known as ‘licensing’29.
An added advantage over other stem cell types is that MSCs are not immunologically active due to low MHC1 and lack of MHCII and co-stimulatory CD80, CD40 and CD86, which protects MSCs from natural killer (NK) cell lysis30. Furthermore, MSCs can inhibit NK and cytotoxic T-cells via various pathways, such as secretion of human leukocyte antigen G5, leukemia inhibitor factor (LIF) and IFNg31-33. More specifically, MSCs induce T-cell apoptosis, which enables macrophages to produce TGFb, thus promoting generation of regulatory T-cells and macrophage phenotype switching to anti-inflammatory subtypes34-36. These immunomodulatory effects depend on the quantity and type of cytokines present and diminish the risk of immune rejection, making MSCs a viable option in inflammatory conditions and other clinical applications37,38. However, intensity of inflammation regulates MSC-mediated immunomodulation, necessitating a strong patient inflammatory status for optimal efficacy39. Therefore, burn injuries are a potential application for MSCs. The added advantage of using skin MSCs in particular is that these cells can be easily isolated from debrided burn eschar. In the subsequent section, we discuss the isolation and advantage of utilizing BD-MSCs.
Isolation of Mesenchymal Stem Cells from Burn Skin
Debrided burn skin, which is routinely discarded after excision, contains a host of viable cells that have the potential to be extracted and incorporated into skin substitutes. We previously demonstrated that viable BD-MSCs can be isolated from the dermal component of surgically debrided burn skin (Figure 1). BD-MSCs can be extracted easily either using an enzymatic or a conventional method. For the former, we homogenized fresh tissue and incubated with collagenase I. For the latter, we washed tissue in PBS with 1% Ab/Am, cut tissue into 1cm squares and placed in high glucose DMEM supplemented with 10% FBS and 1% Ab/Am, and allowed cells to adhere to the surface. Isolated cells were characterized using flow cytometry (CD73+CD105+CD34-CD45-), and multipotency was confirmed by adipogenic, chondrogenic, and osteogenic differentiation. For the in vivo murine model, Matrigel containing 110,000 BD-MSCs were applied directly to the full-thickness punch wound and was subsequently covered with Tegaderm. For porcine experiments, we compared wound healing outcomes with Integra or Integra containing 5,000-400,00 BD-MSCs/cm2 in excised burn wounds.
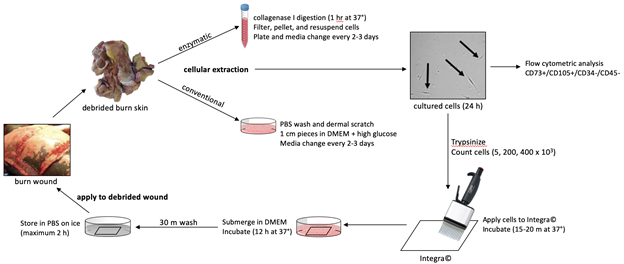
Figure 1: Schematic of the methods and application of BD-MSCs in the clinical setting.
Outcomes with MSCs
To date, there are several studies investigating applications of locally or systemically injected and topical MSCs in animal burn models40. For the purposes of this review, we will highlight studies focused the beneficial effects of MSC-seeded biomaterials (e.g. decellularized tissue extracts, premade porous scaffolds, hydrogel formulations) on burn wound healing as a comparison to our previous work. Several studies in rodent burn models investigated the effect of scaffolds seeded with human MSCs41-44. These studies demonstrated accelerated wound closure in full-thickness burns, with enhanced vascularization, granulation tissue formation, and wound maturity – markers for improved healing40. Other studies investigating BM-MSC-seeded scaffolds in rodent partial-thickness burns showed similar effects45,46. Namely, Guo et al. showed evidence of enhanced re-epithelialization and cellular proliferation coupled with greater blood vessel density, and Yang et al. demonstrated accelerated wound healing and time to closure45,46. Similarly, several porcine studies investigated the effect of scaffolds seeded with autologous, allogeneic, or xenogeneic MSCs to treat deep partial- or full-thickness burns. Clover et al. demonstrated evidence of increased collagen content, epidermal area, and dermal thickness by 14 day post-transplantation, while Liu et al. showed enhanced wound area contraction at 4 weeks after management with an autologous BM-MSC seeded scaffold47,48. Burmeister et al. also demonstrated increased blood vessel size and percentage of biopsy area represented by blood vessels, providing evidence of enhanced angiogenesis with treatment49.
We demonstrated similar results with BD-MSCs, with the added advantage that these cells can be isolated directly from discarded burn tissue. In fact, administration of BD-MSCs in Matrigel in immunodeficient mice enhanced wound closure, reduced granulation tissue size, and reduced the thickness of the keratinocyte layer12. This indicates a potential anti-scarring effect, which is promising due to the fact that burn patients frequently suffer from abnormal scarring. Furthermore, BD-MSC administration promoted an earlier transition to the remodeling phase of healing. Porcine wound models, which resemble human wounding, similarly exhibited an accelerated epithelialization time and greater dermal blood vessel content, another marker of healing12. While this may be a consequence of general wound healing, BD-MSCs may have the potential to directly promote neovascularization. Furthermore, an important consideration of using cell therapy is safety and the potential for tumorigenicity, and we demonstrated no detrimental effects in vitro and in vivo in both murine and porcine wound healing models over 30 days12.
To date, there are few studies regarding MSC application in human burn wound healing, and the current studies vary with regards to the time to first MSC administration (five to 29 days). Rasulov et al. first described the topical application of allogeneic BM-MSCs for management of a patient with extensive, severe burns, demonstrating enhanced skin graft take and neoangiogenesis50. Another case study by Mansilla et al. investigated administration of BM-MSCs in a fibrin matrix spray system for a 30% TBSA full-thickness burn51. The authors demonstrated early “granulation-like tissue” by day 5 post-treatment, with evidence of epithelialization at the wound margins and almost no scarring during the three-year follow-up. However, it is difficult to determine causality in these case reports due to the lack of controls, although these results suggest that MSC application to human burn wounds may be a potential line of investigation. This is especially promising given the effects on wound contracture and scarring. Abo-Elkheir et al. demonstrated decreased contracture and hypertrophic scarring with locally injected autologous BM-MSCs, in addition to fewer late complications52.
In addition to improved healing, there are several other advantages to utilizing BD-MSCs. Compared to embryonic stem cells, there are no ethical obstacles to BD-MSC extraction, and discarded tissue provides an ample source of stem cells. Additionally, isolation of BD-MSCs is non-invasive compared to other sources of MSCs and because these are the patients’ own cells, there is no added concern of immunological rejection. As we demonstrated earlier, BD-MSCs can easily be incorporated into wound coverage materials or scaffolds, providing an easy, cost-effective method for stem cell delivery to the site of injury. However, there are several limitations in our study and potential issues with the clinical use of cultured autologous cells. Firstly, there are regulatory issues associated with the use of cultured autologous cells in general. Culture expansion of cells is considered to be “more than minimal” manipulation, and these products are classified as medicinal products or biologics that must comply with Good Manufacturing Practice (GMP) guidelines53. This introduces additional regulatory challenges prior to clinical implementation, compounded by factors such as variations between clinical sites53.
Additionally, although we demonstrate no detrimental effects with BD-MSCs, several studies suggest potential adverse affects with MSC treatment54. Also, we did not investigate alternate routes of administration such as local subcutaneous or intradermal injection, which shows some promise in several murine and porcine studies40. Furthermore, although we detected human BD-MSCs in murine wound tissue after wound closure, it is unclear whether these cells remained in their MSC-state or differentiated into skin cells. While we provided evidence of MSC survival in burn tissue, additional research is needed to determine how these cells survive. We postulate that this population of stem cells may differ due to their ability to resist heat via activation of cellular stress responses. Post-burn changes include altered mitochondrial dynamics (e.g. enhanced uncoupling), and previous studies have shown that mitochondrial function influences cellular renewal and differentiation55. In fact, mitochondrial fusion is needed to promote stem cell differentiation and therefore, post-burn mitochondrial dysregulation could promote resistance to differentiation in these populations. Although this is speculative and further work is still needed to elucidate their underlying pro-healing mechanisms, BD-MSC-embedded scaffolds are a promising therapeutic option for burn wound management.
Concluding Remarks
Although advances in wound care have improved burn patient outcomes, severe burns are still associated with significant morbidity and mortality. Currently, excision and grafting is the gold standard for burn patient management. However, a paucity of healthy skin in severe burns limits efficacy of autografting. Therefore, utilizing cell-based therapies such as biomaterial sheets with MSCs may be an attractive option in wound management (Table 1)
Table 1. Advantages and disadvantages of topical cell-based therapies
|
Cell-Based Therapy |
Advantages |
Limitations |
|
BD-MSCs |
Can isolate easily from discarded tissue12 Low chance of immunological rejection12 Same as other sources of MSCs |
Need to identify different characteristics from non-burn MSCs12 |
|
Other sources of MSCs (e.g. bone marrow, adipose) |
Multipotent, self-regenerative capacity Easy to isolate and characterize56 Paracrine secretion of cytokines (e.g. IFNg, TNFa, IL1), growth (e.g. EGF, VEGF) and anti-fibrotic factors26 |
Potentially invasive extraction12 Need to define long-term safety profile and mechanism of action56
|
|
Keratinocyte/ Keratinocyte stem cells |
Small amount of donor skin needed25 Easy to isolate and expand Produce various cytokines needed for healing (e.g. IL1, IL6, TNFa)57 |
Hyperkeratosis and scar contracture25 |
|
Fibroblasts |
Maintain cell viability when cryopreserved Produce key ECM* proteins (e.g. collagens, laminins, fibronectins)57,58 Can be induced into pluripotent stem cells56 |
Heterogenous populations58 Efficacy not clearly established in vivo59
|
*ECM=extracellular matrix
Conflict of Interest
The authors declare no conflicts of interest.
Source of Funding
This study was supported by Canadian Institutes of Health Research #123336. CFI Leader’s Opportunity Fund: Project #25407 NIH RO1 GM087285-01
References
- Pereira CT, Herndon DN. The pharmacologic modulation of the hypermetabolic response to burns. Adv Surg. 2005; 39: 245–261.
- Scott-Conner CE, Meydrech E, Wheeler WE, et al. Quantitation of rate of wound closure and the prediction of death following major burns. Burns Incl Therm Inj. 19988; 14: 373-378.
- Ziegler B, Hirche C, Horter J, et al. In view of standardization part 2: Management of challenges in the initial treatment of burn patients in Burn Centers in Germany. Burns. 2017; 43: 318-325.
- Peck MD, Kruger GE, van der Merwe AE, et al. Burns and fires from non-electric domestic appliances in low and middle income countries part I. the scope of the problem. Burns. 2008; 34: 303-311.
- Wehrens KM, Arnoldussen CW, Booi DI, et al. Clinical evaluation of wound healing in split-skin graft donor sites using microscopic quantification of reepithelialization. Adv Skin Wound Care. 2016; 29: 254-260.
- Martindale RG, McClave SA, Vanek VW, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine and American Society for Parenteral and Enteral Nutrition: Executive Summary. Crit Care Med. 2009; 37(5): 1757-1761.
- Jeschke MG, Kalmolz LP, Shahrokhi S. Burn Care and Treatment. Toronto, Canada: Springer Vienna; 2013.
- Mullen JL, Buzby GP, Waldman MT, et al. Prediction of operative morbidity and mortality by preoperative nutritional assessment. Surg Forum. 1979; 30: 80-82.
- Jones SG, Edwards R, Thomas DW. Inflammation and wound healing: the role of bacteria in the immuno-regulation of wound healing. Int J Low Extrem Wounds. 2004; 3(4): 201-208.
- Edwards R, Harding KG. Bacteria and wound healing. Curr Opin Infect Dis. 2004; 17(2): 91-96.
- Branski LK, Al-Mousawi A, Rivero H, et al. Emerging infections in burns. Surg Infect. 2009; 10: 389–97.
- Amini-Nik S, Reinhard D, Eylert G, et al. Stem cells derived from burned skin – The future of burn care. EBioMedicine. 2018; 37: 509-520.
- Healy C, Greig AV, Murphy AD, et al. Prospective randomized controlled trial: fibrin sealant reduces split skin graft donor-site pain. Plast Reconstr Surg. 2013; 132: 139e-146e.
- Kearney JN. Clinical evaluation of skin substitutes. Burns. 2001; 27: 545-551.
- Tompkins RG, Burke JF. Progress in burn treatment and the use of artificial skin. World J Surg. 1990; 14: 819-824.
- Yannas IV, Burke JF. Design of an artificial skin. I. Basic design principles. J Biomed Mater Res. 1980; 14: 65-81.
- Hart DW, Wolf SE, Chinkes DL, et al. Effects of early excision and aggressive enteral feeding on hypermetabolism, catabolism, and sepsis after severe burn. J Trauma. 2003; 54(4): 755-764.
- Williams FN, Herndon DN, Jeschke MG. The Hypermetabolic Response to Burn Injury and Interventions to Modify This Response. Clin Plast Surg. 2009; 36(4): 583-596.
- Peck MD. Epidemiology of burns throughout the world. Part I: distribution and risk factors. Burns. 2011; 37: 1087-1100.
- Ong YS, Samuel M, Song C. Meta-analysis of early excision of burns. Burns. 2006; 32(2): 145-150.
- Vinita P, Khare NA, Chandramouli M, et al. Comparative analysis of early excision and grafting vs delayed grafting in burn patients in a developing country. J Burn Care Res. 2014; 1.
- Still JM, Law EJ. Primary excision of the burn wound. Clin Plast Surg. 2000; 27(1): 23-47.
- Rousseau AF, Massion PB, Laungani A, et al. Toward targeted early burn care: lessons from a European survey. J Burn Care Res. 2014; 35(4): e234-239.
- Posluszny JA, Gamelli RL. Anemia of thermal injury: combined acute blood loss anemia and anemia of critical illness. J Burn Care Rehabil. 2010; 31(2): 229-242.
- Mcheik JN, Barrault C, Levard G, et al. Epidermal Healing in Burns: Autologous Keratinocyte Transplantation as a Standard Procedure: Update and Perspective. Plast Reconstr Surg Glob Open. 2014; 2(9): e218.
- Baraniak PR, McDevitt TC. Stem cell paracrine actions and tissue regeneration. Regen Med. 2010; 5(1): 121-143.
- Halim AS, Khoo TL, Mohd Yussof SJ. Biologic and synthetic skin substitutes: An overview. Indian J Plast Surg. 2010; 43: S23-S28.
- Han Y, Xuezhou L, Zhang Y, et al. Mesenchymal Stem Cells for Regenerative Medicine. Cells. 2019; 8(8): 886.
- Krampera M. Mesenchymal stromal cell ‘licensing’: a multistep process. Leukemia. 2011; 25: 1408-1414.
- Rasmusson I, Ringdén O, Sundberg B, et al. Mesenchymal stem cells inhibit the formation of cytotoxic T lymphocytes, but not activated cytotoxic T lymphocytes or natural killer cells. Transplantation. 2003; 76(8): 1208-1213.
- Selmani Z, Naji A, Zidi I, et al. Human leukocyte antigen-G5 secretion by human mesenchymal stem cells is required to suppress T lymphocyte and natural killer function and to induce CD4+CD25highFOXP3+ regulatory T cells. Stem Cells. 2008; 26(2): 212-222.
- Nasef A, Mazurier C, Bouchet S, et al. Leukemia inhibitory factor: Role in human mesenchymal stem cells mediated immunosuppression. Cell Immunol. 2008; 253(1-2): 16-22.
- Shen H, Wang Y, Jin Y, et al. A critical role of IFNgamma in priming MSC-mediated suppression of T cell proliferation through up-regulation of B7-H1. Cell Res. 2008; 18(8): 846-857.
- Akiyama K, Chen C, Wang DD, et al. Mesenchymal-stem-cell-induced immunoregulation involves FAS-ligand-/FAS-mediated T cell apoptosis. Cell Stem Cell. 2012; 10(5): 544-555.
- Németh K, Leelahavanichkul A, Yuen PST, et al. Bone marrow stromal cells attenuate sepsis vis prostaglandin E(2)-dependent reprogramming of host macrophages to increase their interleukin-10 production. Nat Med. 2009; 15(1): 42-49.
- Abumaree MH, Al Jumah MA, Kalionis B, et al. Human placental mesenchymal stem cells (pMSCs) play a role as immune suppressive cells by shifting macrophage differentiation from inflammatory M1 to anti-inflammatory M2 macrophages. Stem Cell Rev Rep. 2013; 9(5): 620-641.
- Mansilla E, Marin GH, Drago HE, et al. Human mesenchymal stem cells are tolerized by mice and improve skin and spinal cord injuries. Transplant Proc. 2005; 37(10): 292-294.
- Falanga V, Iwamoto S, Chartier M, et al. Autologous bone marrow-derived cultured mesenchymal stem cells delivered in a fibrin spray accelerate healing in murine and human cutaneous wounds. Tissue Eng. 2007; 13(6): 1299-1312.
- Wang Y, Chen X, Cao W, et al. Plasticity of mesenchymal stem cells in immunomodulation: pathological and therapeutic implications. Nat Immunol. 2014; 15(11): 1009-1016.
- Rangatchew F, Vester-Glowinski P, Rasmussen BS, et al. Mesenchymal stem cell therapy of acute thermal burns: A systematic review of the effect on inflammation and wound healing. Burns, in press.
- Shumakov VI, Onishchenko NA, Rasulov MF, et al. Mesenchymal bone marrow stem cells more effectively stimulate regeneration of deep burn wounds than embryonic fibroblasts. Bull Exp Biol Med. 2003; 1363: 192-195.
- Rasulov MF, Vasilenko VT, Zaidenov VA, et al. Cell transplantation inhibits inflammatory reaction and stimulates repair processes in burn wound. Bull Exp Biol Med. 2006; 142: 112-115.
- Pourfath MR, Behzad-Behbahani A, Hashemi SS, et al. Monitoring wound healing of burn in rat model using human Wharton’s jelly mesenchymal stem cells containing cGFP integrated by lentiviral vectors. Iran J Basic Med Sci. 2018; 21: 70-76.
- Alapure BV, Lu Y, He M, et al. Accelerate healing of severe burn wounds by mouse bone marrow mesenchymal stem cell-seeded biodegradable hydrogel scaffold synthesized from arginine-based poly(ester amide) and chitosan. Stem Cells Dev. 2018; 27: 1605-1620.
- Guo X, Xia B, Lu XB, et al. Grafting of mesenchymal stem cell-seeded small intestinal submucosa to repair the deep partial-thickness burns. Connect Tissue Res. 2016; 57: 388-397.
- Yang Y, Zhang W, Li Y, et al. Scalded skin of rat treated by using fibrin glue combined with allogeneic bone marrow mesenchymal stem cells. Ann Dermatol. 2014; 26: 289-295.
- Clover AJP, Kumar AHS, Isakson M, et al. Allogeneic mesenchymal stem cells, but not culture modified monocytes, improve burn wound healing. Burns. 2015; 41: 548-557.
- Liu P, Deng S, Han T, et al. Tissue-engineered skin containing mesenchymal stem cells improves burn wounds. Artif Organs. 2008; 32: 925-931.
- Burmeister DM, Stone R, Wrice N, et al. Delivery of allogeneic adipose stem cells in polyethylene glycol-fibrin hydrogels as an adjunct to meshed autografts after sharp debridement of deep partial thickness burns. Stem Cells Transl Med. 2018; 7: 360-372.
- Rasulov MF, Vasilchenkov AV, Onishchenko NA, et al. First experience of the use bone marrow mesenchymal stem cells for the treatment of a patient with deep skin burns. Bull Exp Biol Med. 2005; 139: 141-144.
- Mansilla E, Marin GH, Berges M, et al. Cadaveric bone marrow mesenchymal stem cells: first experience treating a patient with large severe burns. Burn Trauma. 2015; 3: 17.
- Abo-Elkheir W, Hamza F, Elmofty AM, et al. Role of cord blood and bone marrow mesenchymal stem cells in recent deep burn: a case-control prospective study. Am J Stem Cells. 2017; 6: 23-35.
- Eaker S, Armant M, Brandwein H, et al. Concise Review: Guidance in Developing Commercializable Autologous/Patient-Specific Cell Therapy Manufacturing. Stem Cells Transl Med. 2013; 2(11): 871-883.
- Zhang T, Lee YW, Rui YF, et al. Bone marrow-derived mesenchymal stem cells promote growth and angiogenesis of breast and prostate tumors. Stem Cell Res Ther. 2013; 4: 70.
- Deng H, Takashima S, Paul M, et al. Mitochondrial dynamics regulates Drosophila intestinal stem cell differentiation. Cell Death Discov. 2018; 4: 81.
- Otero-Vinas M, Falanga V. Mesenchymal Stem Cells in Chronic Wounds: The Spectrum from Basic to Advanced Therapy. Adv Wound Care (New Rochelle). 2016; 5(4): 149-163.
- You HJ, Han SK. Cell Therapy for Wound Healing. J Korean Med Sci. 2014; 29(3): 311-319.
- Pourmoussa A, Gardner DJ, Johnson MB, et al. An update and review of cell-based wound dressings and their integration into clinical practice. Ann Transl Med. 2016; 4(23): 457.
- desJardins-Park HE, Foster DS, Longaker MT. Fibroblasts and wound healing: an update. Regen Med. 2018; 13(5): 491-495.
